











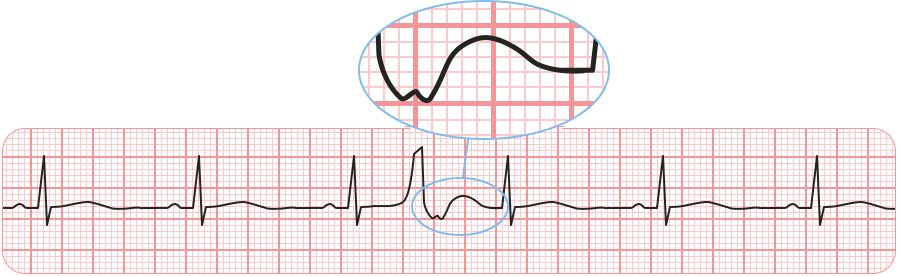

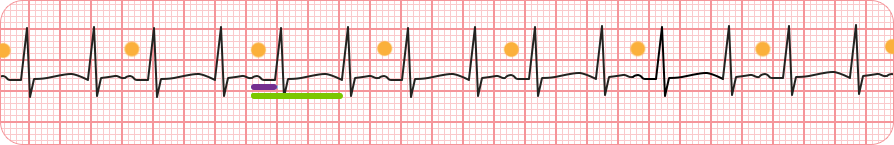
Double Firing 🔥🔥 #epCINRE #EPeeps
— Peter Blahút (@PeterBlahut) February 29, 2024
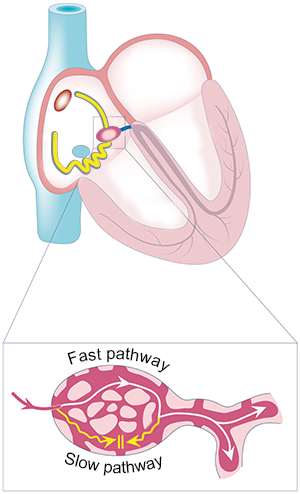
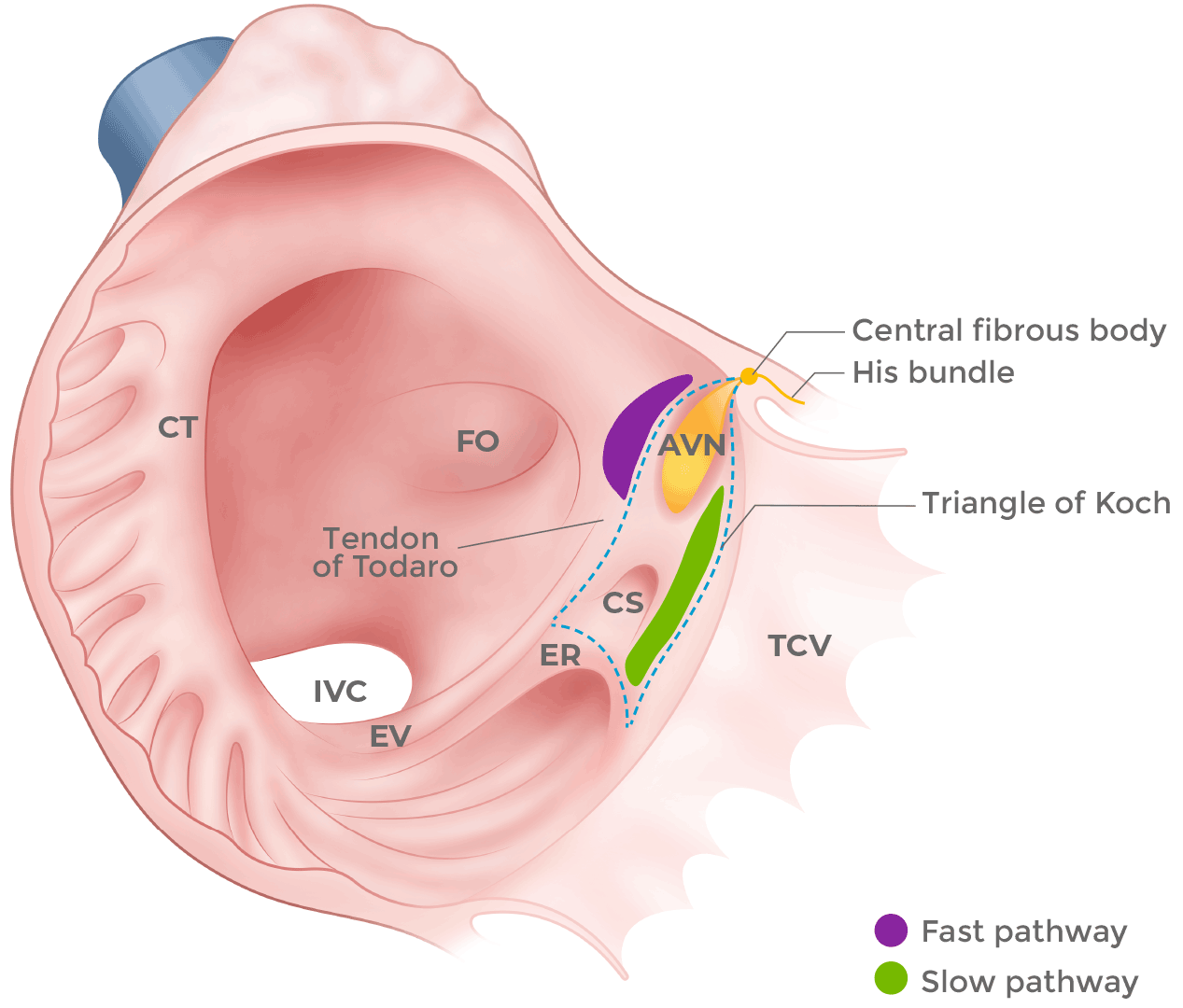
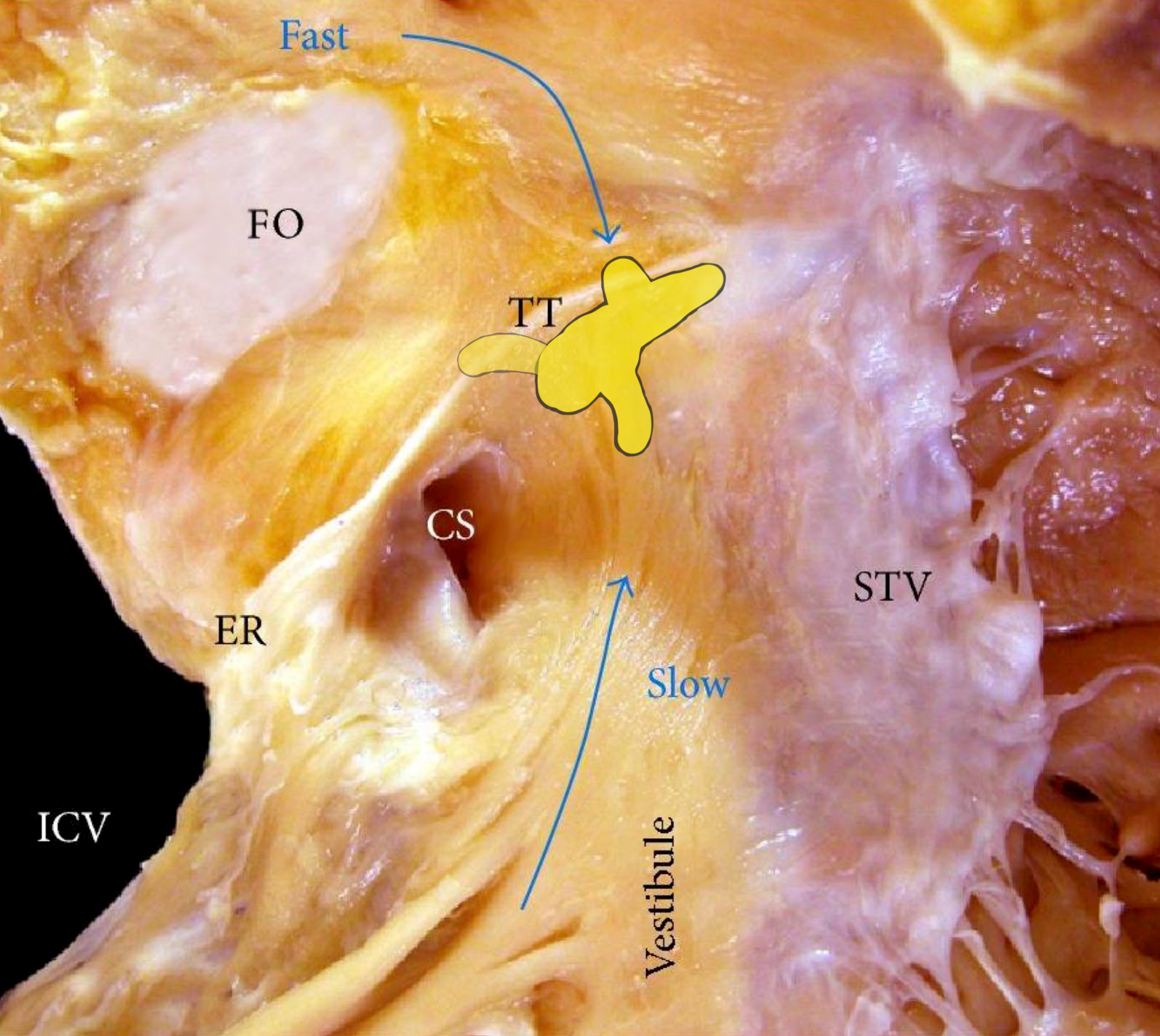
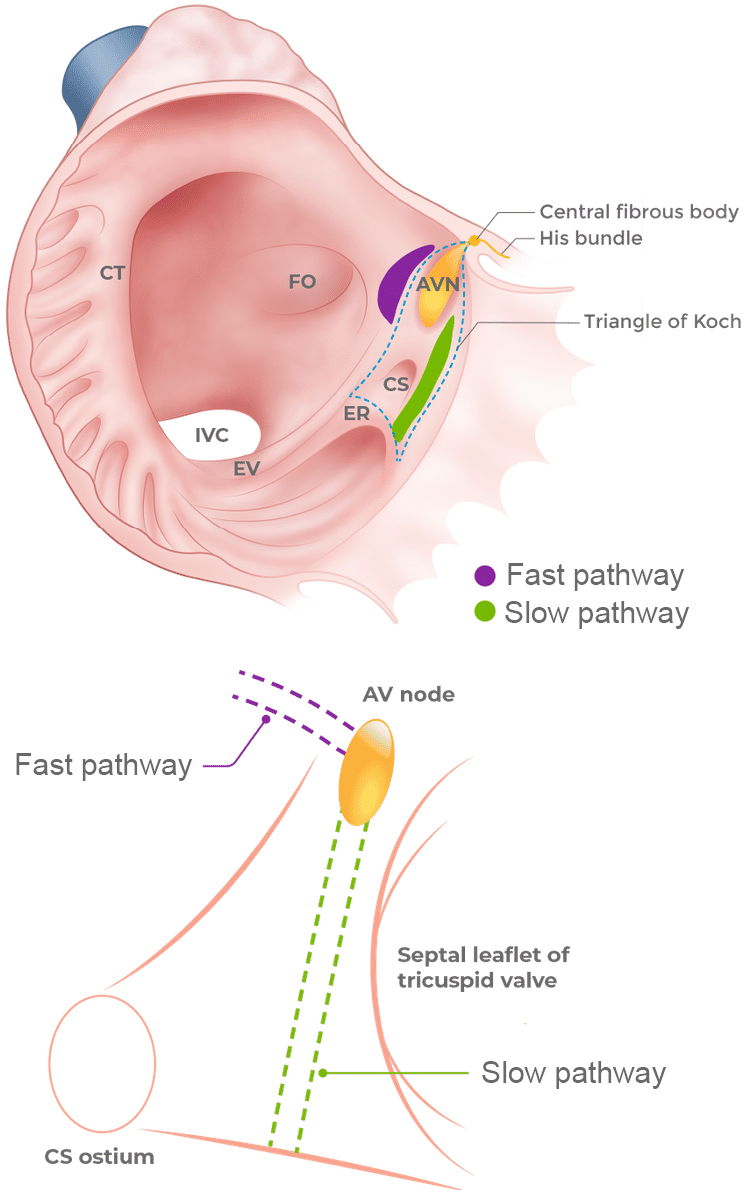
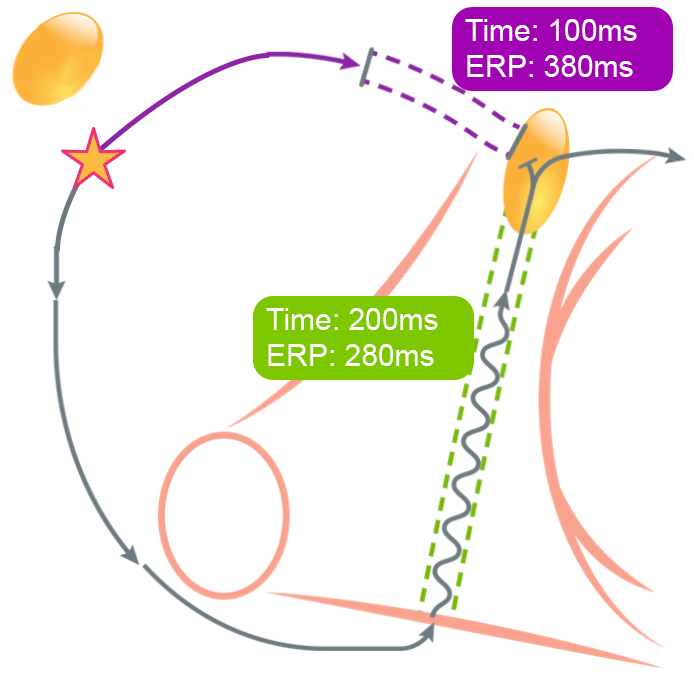
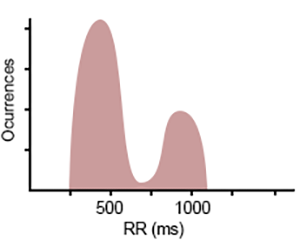
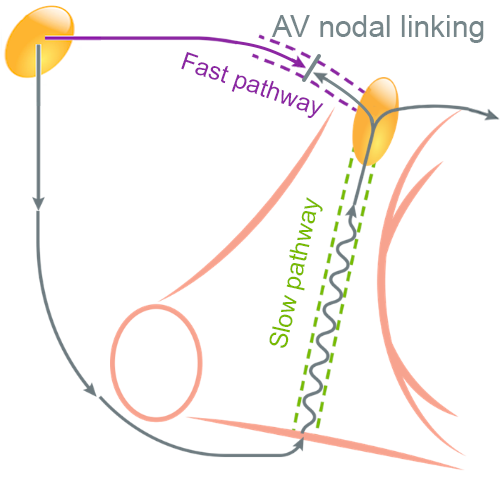
1⃣ Dual AVN physiology affects 10-35% population
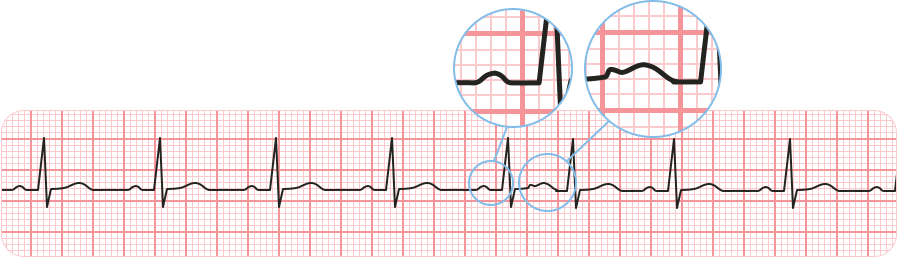
2⃣ Occurs if the slow pathway is very slow
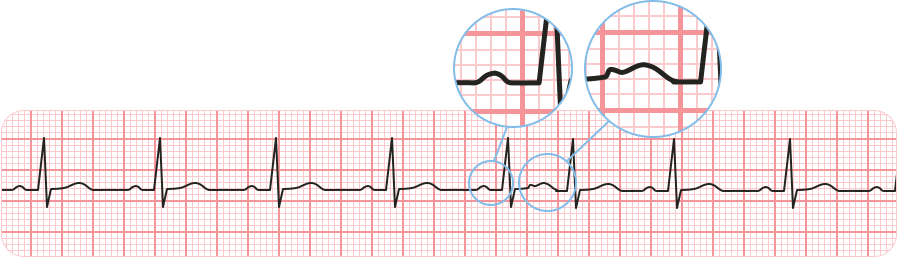
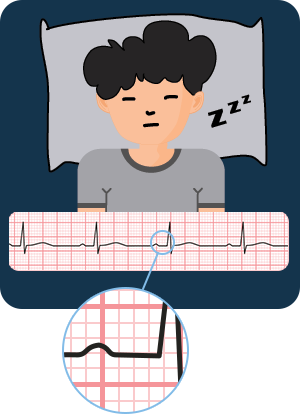
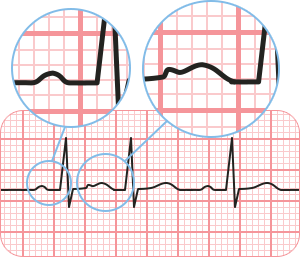
3⃣ #ECG P -> 2 QRS
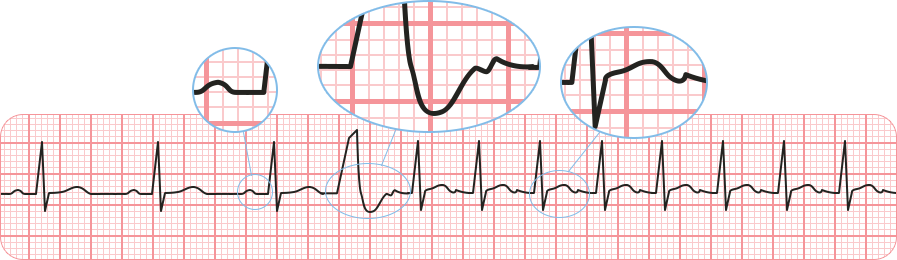
4⃣ Misdiagnosed as AF or PAC
5⃣ DAVNNT is continuing 🔥🔥
👉 Dual AVN Non-Reentrant Tachycardia
6⃣ Treatment: Slow pathway RFA 🥳🎉💘 pic.twitter.com/HKJZp0Ag8Q